Be it a tertiary care center or a primary health center, sore throat is the most common disease that a clinician will encounter during the OP hours. Sore throat, Upper Respiratory Tract Infection (URTI) for the medicos, is an infection of the pharynx and usually, it is a self-limiting disease. Out of 100 patients clinicians attend, minimum 40 will be complaining about sore throat and it is contagious too. The classical teaching about sore throat is that with treatment it will subside by 7 days and by one week sans it. The causative organisms are innumerable, however, the list predominantly contains viruses like Adenovirus, Influenza, Parainfluenza, Measles, Rhinovirus, etc. and consequently the need for antibiotics in sore throat patients is minimal(1,2). Bacterial sore throats are statistically less likely than viral causes and this is a fact that needs to be there in the minds of all practicing clinicians.
As the causative organisms are viruses in the majority of the cases, antibiotics are not required for treatment and this fact has to be conveyed to the patient as well so that they don’t purchase over the counter antibiotics. A bronchodilator (medications which widens your airway) like salbutamol and a nasal decongestant (which clears the nasal secretions) like saline nasal drops are sufficient to provide symptomatic relief for the patients. Notwithstanding the symptoms relief, there is no conclusive evidence to suggest that these medications shorten the duration of disease (3,4). Physicians, due to multiple reasons including pressure from parents, prescribe antibiotics for sore throat and common cold which typically do not benefit from antimicrobials(5).
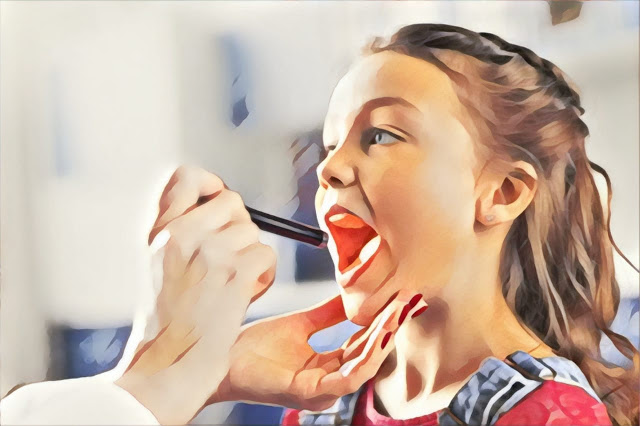
Certain scoring systems like Centor and McIssac criteria(6), which are scoring systems to calculate the risk of bacterial infections in a case of sore throat based on the symptom profile of the patient, are formulated for helping the physician to decide on antibiotics. The importance in scoring systems lies in the fact that we don’t have enough fast and economically feasible diagnostic tests to find out the organisms causing the sore throat. Antibiotic therapy for bacterial sore throat is crucial in the pediatric population as Group-A Beta Hemolytic Streptococci, a Gram-positive bacteria belonging to the Streptococci family which can cause Rheumatic fever, is the most common bacterial pathogen associated with a sore throat. Rheumatic fever is a disorder that presents with fever and joint pain, which can potentially affect the heart leading to morbidity and mortality.
Acute pharyngitis is caused by viruses in more than 70 percent of cases in young children. Mild pharyngeal redness and swelling and tonsil enlargement are typical. Streptococcal infection is rare in children under five and more common in older children.
– Eric et al (1).
If at all there is an indication for antimicrobial therapy, the first choice should be a Penicillin antibiotic like Amoxicillin or Penicillin V as they can cover Streptococci bacteria. Nevertheless, some physicians prescribe Azithromycin alone or in combination with Amoxicillin for sore throat and such habits are against the antibiotic stewardship, a practice that we follow to preserve the efficacy of antibiotics against pathogens. Azithromycin has inferior activity against the Gram-positive organisms as compared to the Penicillin group of antibiotics and its efficacy is better for atypical microorganisms like Chlamydia, Mycoplasma, and Legionella. It must be kept in mind that Azithromycin is one of the drugs that we use for resistant typhoid and hence, we should preserve its sensitivity. Mycoplasma can cause a sore throat but the incidence is far less in comparison with Streptococci and usually, Mycoplasma affects the upper airway along with the lower airway.
It has been stated in standard textbooks like Nelson Textbook of Pediatrics that the use of Azithromycin is justified only as a second line after Penicillin for sore throat. WHO-AWARE classification places Azithromycin in ‘WATCH’ group of antibiotics and this means that it has to be used judiciously as a second-line agent(7). Due to indiscriminate use in peripheral centers, Azithromycin resistance has developed to a great extent and at my center, we are now using Doxycycline to cover the atypical organisms causing pneumonia. Previously, we used to use Azithromycin whenever we had suspicion about the atypical pneumonia.

Despite having an innocuous course, URTI can harm our antibiotic reserves due to the non-judicious use of antibiotics for its treatment. Always remember that we don’t need to fire an AK-47 to get rid of a rat from warehouse.
References
1. Simoes EAF, Cherian T, Chow J, Shahid-Salles SA, Laxminarayan R, John TJ. Acute Respiratory Infections in Children.
2. Denny FW. The clinical impact of human respiratory virus infections. Am J Respir Crit Care Med. 1995 Oct;152(4 Pt 2):S4–12.
3. Schroeder K, Fahey T. Over-the-counter medications for acute cough in children and adults in ambulatory settings. Cochrane Database Syst Rev. 2004 Oct 18;(4):CD001831.
4. Im P, Ke Y, Kr C, Ml S, Hs M, Lc C, et al. Effect of dextromethorphan, diphenhydramine, and placebo on nocturnal cough and sleep quality for coughing children and their parents Available from: https://pubmed.ncbi.nlm.nih.gov/15231978/
5. Ac N, R G, Jf S, Ma S. Antibiotic prescribing for children with colds, upper respiratory tract infections, and bronchitis [Internet]. Available from: https://pubmed.ncbi.nlm.nih.gov/9516004/
6. Fine AM, Nizet V, Mandl KD. Large-Scale Validation of the Centor and McIsaac Scores to Predict Group A Streptococcal Pharyngitis. Arch Intern Med. 2012 Jun 11;172(11):847–52.
7. WHO | WHO releases the 2019 AWaRe Classification Antibiotics [Internet]. WHO. [cited 2020 Oct 14]. Available from: http://www.who.int/medicines/news/2019/WHO_releases2019AWaRe_classification_antibiotics/en/
Please give your valuable feedback as comments in the comments section. You can also use the floating messenger button to contact me through Facebook.